Technology
What is Blood saturation?
Blood Saturation is an index given to the amount of Hemoglobin in percentage, that is being used to carry oxygen. Hemoglobin exists inside every red blood cell, and when the blood cell enters the lung, oxygen chemically attaches itself to hemoglobin. Such molecule is called Oxyhemoglobin (Hb02). When calculating Hemoglobin saturation levels, the HbO2 molecules are divided by the sum total amount of Hb molecules, and multiplied by a 100. the result figure is the Hemoglobin Saturation Index.
Many respiratory diseases occur due to low hemoglobin Saturation levels – though the blood flows well, hemoglobin cannot carry oxygen at full capacity. If low hemoglobin levels are accompanied by other medical conditions such as, arthrosclerosis, heart problems, airway congestion etc', the oxygen levels in the blood can drop sharply overtime, and can endanger the patient's life.
Therefore. it is very important to know Hemoglobin saturation levels of the patient, constantly, in order for the doctors to know in advance, that something is wrong.
The Fingertip Pulse Oximeter is light weighted, easy to use, consumes low amounts of energy and isn't susceptible to movement. All the patient has to do is place one finger (of his choice) into the FOS2. inside the FOS2 there is a photoelectric sensor, which diagnoses both heart rate and Hemoglobin saturation levels. Both indexes are displayed on the screen immediately. The FOS2 passed rigorous clinical experiments, and was found to be highly accurate.

Buy Now
HKD$3000HKD$2500
What exactly does the pulse oximeter measure?
Blood carries oxygen in two forms, the majority is bound to hemoglobin (oxyhemoglobin) and the rest is dissolved in the aqueous phase of blood (the plasma).
The pulse oximeter measures the saturation of hemoglobin with oxygen. This is expressed as a percent saturation. Each gram of normal hemoglobin can hold 1.34 milliliters of oxygen. The dissolved fraction is dependent upon the partial pressure of oxygen. As the partial pressure increases, the dissolved fraction of oxygen increases.
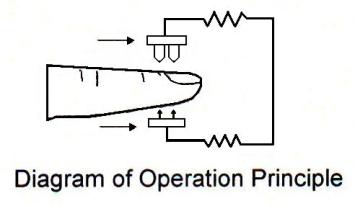
For each 1mmHg pressure of oxygen partial pressure0.003 milliliters dissolves in the plasma. So under normal conditions each 100-ml of blood contains about 20 ml of oxygen bound to hemoglobin and about 0.3 ml dissolved in plasma, The dissolved fraction is available to tissues first, and then the fraction bound to hemoglobin. So as tissues metabolize oxygen, or if oxygen becomes difficult to pink up through the lungs the dissolved oxygen and the hemoglobin – bound oxygen will eventually become depleted. The dissolved oxygen can be measured by arterial blood gas analysis but this is not yet practical for field application. This fraction is not measured by pulse oximetry. The pulse oximeter waits to sense the pulse of capillary blood from side of the capillaries, then using two different wavelengths of light calculates the percent of oxyhemoglobin from the total hemoglobin present. If oxygen transfer across the lungs or lung function is compromised and as tissues continue to metabolize oxygen, the percentage of oxyhemoglobin will decrease. This becomes our quantitative indicator of hypoxia.
(Learn more about Pulse Oximetry)
Uses of pulse oximetry
Simple, portable "all-in-one" monitor of oxygenation, pulse rate and rhythm regularity, suitable for "field" use.
As a safe, non-invasive monitor of the cardio-respiratory status of high-dependency patients - in the emergency department, during general and regional anaesthesia, postoperatively and in intensive care. This includes procedures such as endoscopy, where often frail patients are given sedative drugs such as midazolam. Pulse oximeters detect the presence of cyanosis more reliably than even the best doctors when using their clinical judgement.
During the transport of patients - especially when this is noisy - for example in aircraft, helicopters or ambulances. The audible tone and alarms may not be heard, but if a waveform can be seen together with an acceptable oxygen saturation, this gives a global indication of a patient's cardio-respiratory status.
To assess the viability of limbs after plastic and orthopaedic surgery and, for example, following vascular grafting, or where there is soft tissue swelling or aortic dissection. As a pulse oximeter requires a pulsatile signal under the sensor, it can detect whether a limb is getting a blood supply.
As a means of reducing the frequency of blood gas analysis in intensive care patients- especially in paediatric practice where vascular (arterial) access may be more difficult.
To limit oxygen toxicity in premature neonates supplemental oxygen can be tapered to maintain an oxygen saturation of 90% - thus avoiding the damage to the lungs and retinas of neonates. Although pulse oximeters are calibrated for adult haemoglobin, HbA, the absorption spectra of HbA and HbF are almost identical over the range used in pulse oximetry, so the technique remains reliable in neonates.
During thoracic anesthesia - when one lung is being collapsed down - to determine whether oxygenation via the remaining lung is adequate or whether increased concentrations of oxygen must be given.
Fetal oximetry- a developing technique that uses reflectance oximetry, using LEDs of 735nm and 900nm. The probe is placed over the temple or cheek of the fetus, and needs to be sterile. They are difficult to secure and the readings are variable, for physiological and technical reasons. Hence the trend is more useful than the absolute value.